Newsroom
Health
Uninsured Rates High for Hispanic Children
Utah has Highest Uninsured Rate for Hispanic Children in the Nation
Every child in Utah should have a chance to succeed. When it comes to setting up a child for success, few things matter more than good health. It starts when their mothers get prenatal care. It continues with regular checkups after they are born to treat and, more importantly, prevent illness. Good health care helps children reach important developmental milestones and enter school ready to learn. Coverage is essential to children reaching their full potential. Unfortunately, too many Utah children are uninsured. This is particularly true for Hispanic children in our state.
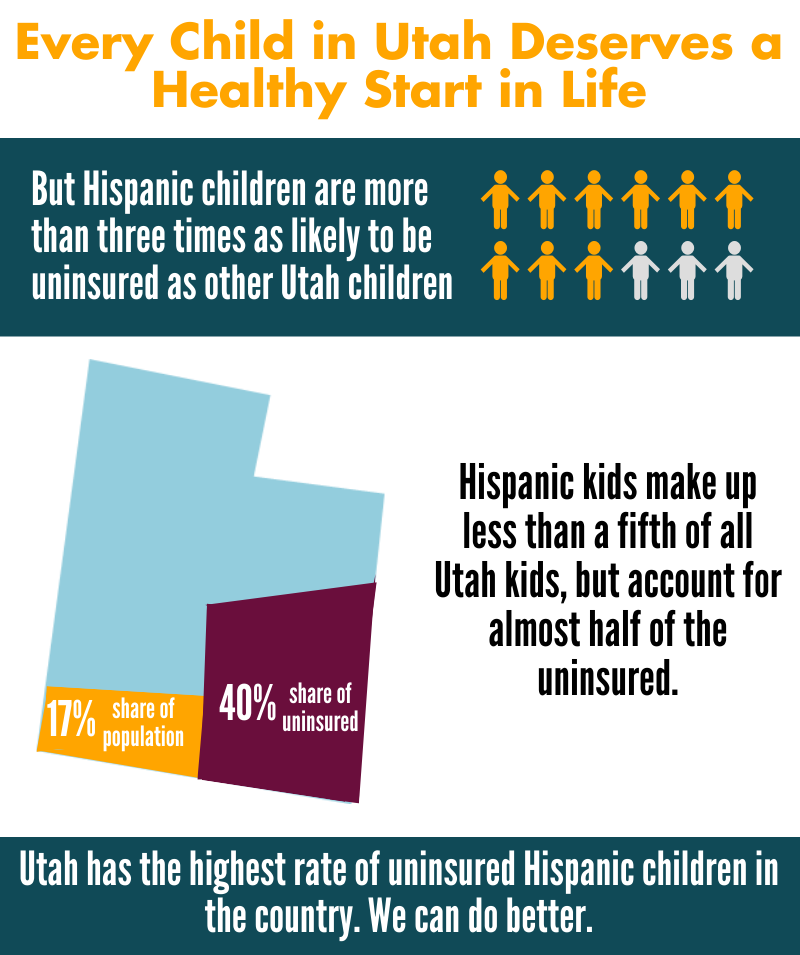 • 22.2% of Hispanic children are uninsured in Utah. This is the highest rate in the nation by far and is twice as high as the national average for Hispanic kids of 11.5%.
• 22.2% of Hispanic children are uninsured in Utah. This is the highest rate in the nation by far and is twice as high as the national average for Hispanic kids of 11.5%.
• 22.2% of Hispanic kids are uninsured compared to only 7% of non-Hispanic children. This 11 percentage point disparity is the largest disparity in the country. Nationally, the average disparity is only 5 percentage points.
• Hispanic children make up 16.9% of Utah’s total child population but account for 39% of the uninsured children in the state. Of the 84,891 uninsured kids in Utah, 33,531 of them are Hispanic.
• Utah’s overall uninsured rate for kids is 9.5%, ranking us 41st (highest being worst) in the country. The national average is 7.1%. If we reduced our Hispanic uninsured rate to the national average of 11.5%, Utah’s overall uninsured rate for kids would drop to 7.5% and Utah would have the 19th best uninsured rate in the country for kids.
If we want more children to succeed in life, we must secure coverage for more of our children, regardless of ethnicity or race. We can begin to remove hurdles facing uninsured Hispanic children and set all of Utah’s children on a path to success by implementing a few first steps:
• Restore outreach funding for Medicaid and CHIP;
• Make it easier for children to keep their health coverage by implementing 12 month continuous eligibility;
• Remove the Medicaid and CHIP five year waiting period that legal immigrant kids must endure before enrolling in these programs.
Printer-friendly version of this factsheet:
Nurse Family Partnership
Nurse Family Partnership (NFP) is a voluntary evidenced-based community health program that provides ongoing home visits (from pregnancy through age 2 of the child) from a registered nurse to low-income, first time mothers to provide the care and support they need to have a healthy pregnancy, be a responsible and caring parent, and to become more economically self-sufficient. A nurse visits the women approximately weekly and bi-monthly during their pregnancy and after birth, and then monthly visits during the first two years of their children’s lives. The program is a two-generation intervention and improves outcomes for both the mother and the child. NFP produces very strong outcomes for very high risk, low-income populations.
Economic analyses performed by the Washington State Institute for Public Policy, the Brookings Institute and the Rand Corporation determined that NFP provides a return on investment for taxpayers of $2.37 to $5.70 (high-risk population) per $1 invested in the program.
Download the printer-friendly report:
Nurse Family Partnership
Proven Outcomes
National outcomes associated with NFP, verified through independently evaluated randomized controlled trials, include long term family improvements in health, child welfare, education and self-sufficiency. When brought to scale, NFP can achieve:
• 23% reduction in smoking during pregnancy
• 26% reduction in pregnancy-induced hypertension
• 18% reduction in first pre-term births
• 58% reduction in infant deaths
• 30% reduction in second teen births
• 37% reduction in childhood injuries treated in emergency departments up to age 2
• 30% reduction in child maltreatment
• 38% reduction in language delay of the child by age 2
• 45% reduction in crimes and arrests, ages 11-17
• 51% reduction in alcohol, tobacco and marijuana use, ages 12-15
• 15% reduction in TANF and Food Stamp payments
• 9% reduction in Medicaid costs through age 1
Locally, Salt Lake County has a small NFP program. In 2012, 10.68% of the comparable Medicaid clients had a preterm delivery, compared to 7.5% of NFP clients, a reduction in incidence of 30%. Preterm babies require expensive medical services and a 30% reduction in incidence results in significant cost savings to Medicaid. In addition, the following outcomes for the mother have been documented in Salt Lake County:
• 52.5% increase in employment of clients younger than 18 after starting the program
• 18.9% increase in employment of clients 18 and older after starting the program
• 40% decrease in maternal smoking
• 50% reduction in reported incidence of domestic violence during pregnancy
Government Cost Savings and Avoidance
The outcomes listed above produce significant cost savings in Medicaid, Criminal Justice, Child Welfare, Food Stamps and TANF. Based on national data, Medicaid is the largest recipient of cost savings per family served (55% of cost savings accrue to Medicaid).
Nurse Family Partnership in Utah
The Office of Home Visiting in the Utah Department of Health received $1,097,713 in federal funding through the Maternal, Infant and Early Childhood Home Visiting (MIECHV) Program for Fiscal Year 2013. Of that, $300,000 was allocated to Nurse Family Partnership to serve 75 families in Salt Lake County (the remaining $700,000 was allocated to Parents as Teachers (PAT) - a home-visiting school readiness program). The average cost per family per year for NFP is $4,000. In 2012 (the most recent data available), 4,867 mothers were eligible for NFP statewide. Based on this, an investment of $19,468,000 would be necessary to serve all eligible families.
Recommendation
Voices for Utah Children recommends an ongoing state appropriation of $2,000,000 per year for Nurse Family Partnership, to serve 500 high risk, low-income first time mother statewide. To date, 21 states have appropriated state funds for NFP and/or home visitation.
More Information
A Two-Generation Strategy: Healthy Parents and Healthy Kids
Healthy Utah Poll Results
 The Healthy Utah Poll was commissioned by a group of Utah civic groups interested in gauging support for Governor Herbert’s Healthy Utah plan. The poll was conducted by Dan Jones & Associates on a sample of 623 Utah voters during May and June, 2014. The full data and methods were then shared with Notalys for independent analysis. Notalys also consulted with the Dan Jones project leader on the development of the survey instrument. This report is the first set of research findings based on the poll. Complete poll results are found in this report along with a description of methods and an analysis of the results. The poll gives a clear and compelling summary of how Utah voters see the Healthy Utah plan, particularly in comparison to other options, such as a full Medicaid Expansion.
The Healthy Utah Poll was commissioned by a group of Utah civic groups interested in gauging support for Governor Herbert’s Healthy Utah plan. The poll was conducted by Dan Jones & Associates on a sample of 623 Utah voters during May and June, 2014. The full data and methods were then shared with Notalys for independent analysis. Notalys also consulted with the Dan Jones project leader on the development of the survey instrument. This report is the first set of research findings based on the poll. Complete poll results are found in this report along with a description of methods and an analysis of the results. The poll gives a clear and compelling summary of how Utah voters see the Healthy Utah plan, particularly in comparison to other options, such as a full Medicaid Expansion.
Download the complete report:
Key findings from the poll analysis
Widespread Support
- When compared with the option of doing nothing, 88% of Utah voters prefer the Healthy Utah plan, and 70% prefer Healthy Utah compared to a full Medicaid expansion.
- Healthy Utah has strong support across the state and among all demographic groups. Support is high for all age, education, race, gender, education and income categories.
No Partisan Divide
- Conservative Republicans support Healthy Utah. Among voters who identify as Republicans, 64% of those who are “very conservative” support the Governor’s plan, while just 13% oppose the plan.
- In general, support among Republicans is higher for Healthy Utah than it is among Democrats, since more Democrats favor Medicaid expansion.
Support for Affordable Health Care
- About 9% of likely voters are currently uninsured, even after healthcare.gov went into effect. A majority (54%) of voters know someone who is uninsured.
- Utahns think health insurance is very important, and, more surprisingly, 83% believe “all legal Utah residents should have access to affordable health insurance.”
- Utah voters believe that individual responsibility is important when it comes to insurance, but they are also supportive of government assistance for those who cannot afford coverage. Of the
- 65% of voters who agree that “individuals and families should generally be responsible for meeting their own healthcare needs,” 80% also agree with the statement that “individuals who are unable to afford health insurance should receive help from government sources.”
- Utahns are not opposed to a federal role in health care. 71% believe it is appropriate for the state to accept federal assistance in health care.
Support for Healthy Utah Plan Features
- A significant majority of voters are interested in the issue of health care, but only about 40% have heard of the new Healthy Utah plan thus far. When the details of the plan are provided, voters are in strong support.
- Utah voters strongly support the individual features of the Healthy Utah plan. Respondents say that the following features of the plan make them more likely to support it than they would otherwise:
- 59% are more likely to support the plan because it requires individuals to pay premiums and co‐pays (10% are less likely).
- 59% are more likely to support the plan because it provides private health insurance for people with low incomes rather than enrolling them in traditional Medicaid (14% are less likely).
- 68% are more likely to support the plan because it allows greater flexibility for how Utah spends federal dollars than allowed under traditional Medicaid (10% are less likely).
Opposed to Inaction
- The strongest consistency in the poll is that voters are very opposed to the status quo of doing nothing. Democrats are more inclined to do a Medicaid expansion, while Republicans support Governor Herbert’s plan. But both groups oppose the status quo. In a three‐way comparison, only 6% of the state voters prefer doing nothing.
- If Healthy Utah is rejected by federal officials, 65% would support a new Utah‐specific solution, and 28% support a Medicaid expansion. Only 7% would favor doing nothing.
- And, 54% of voters indicate they would be more likely to vote for legislators who support Healthy Utah. Only 14% indicate they would be less likely to vote for a legislator who supported the plan.
Poll Take‐Aways
- Utahns are overwhelmingly supportive of the features of Governor Herbert’s Healthy Utah plan.
- Utahns value individual responsibility, but both Republicans and Democrats are strongly supportive of a government role in assisting low‐income individuals to obtain health insurance.
- What Utahns are against, more than anything, is doing nothing.