Utah FAQ’s
What is 12-month continuous eligibility for children on Medicaid?
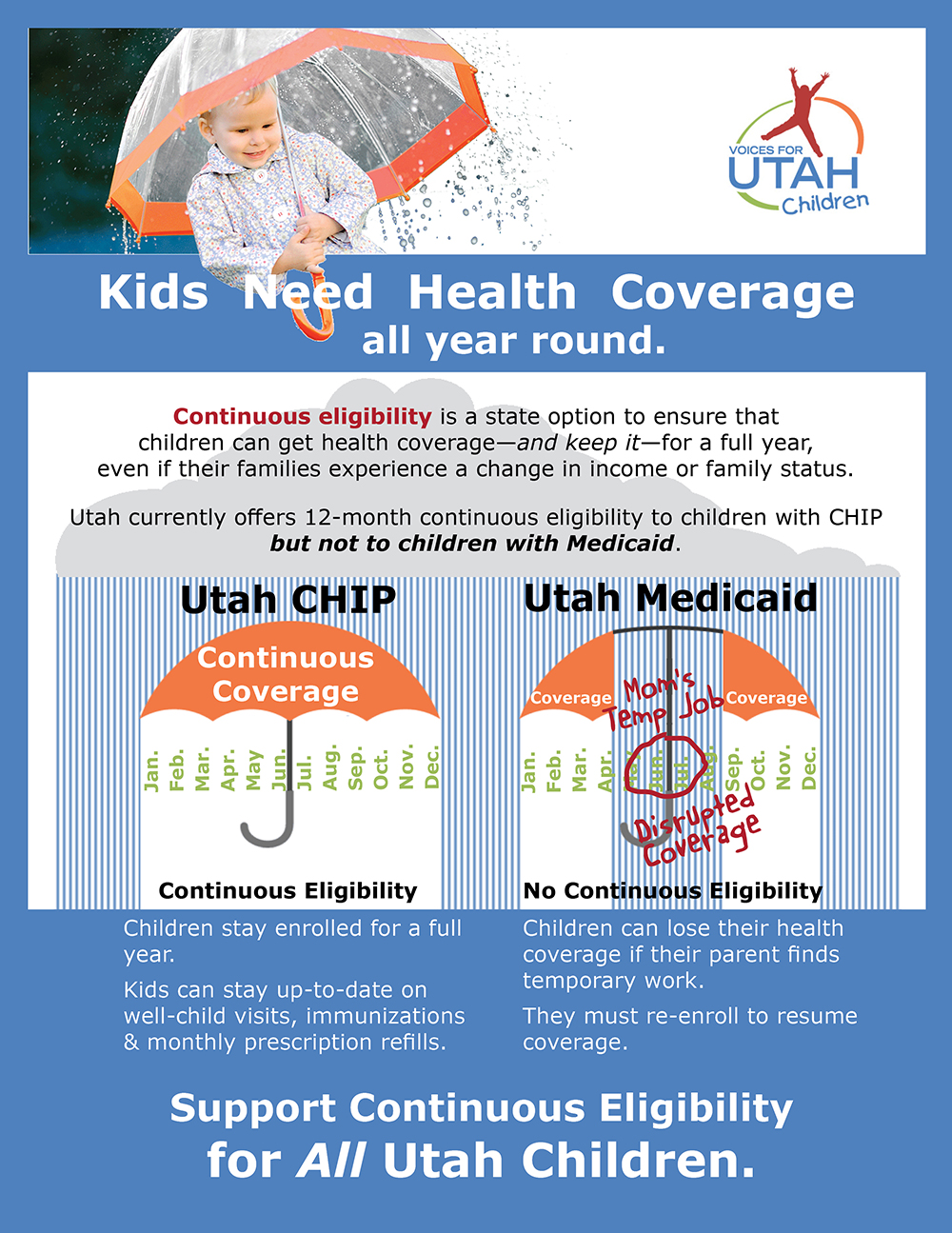
Continuous eligibility is a state option that allows children, up through age 18, to maintain Medicaid coverage throughout the year, even if families experience a change in income or family status. By implementing continuous eligibility policies, a state ensures that for 365 days a year children get—and keep—health coverage.
What is churn?
“Churning” is when children are disenrolled in a public health insurance program and then re-enrolled after only a brief time without public insurance (2-6 months). “Churn” is the on-and-off-and-on pattern of enrollment that may be unrelated to actual eligibility status.
How does 12-month continuous eligibility affect families and children?
When children are enrolled in a program for 12 continuous months, they are less likely to lose their insurance coverage and more likely to experience continuity of care. In many cases, families must dis-enroll from Medicaid after securing unexpected temporary or seasonal work. When the short-term job ends, they must re-enroll in benefits. This creates an unnecessary burden for families. Parents are penalized for trying to improve their family’s economic circumstances through temporary or seasonal work.
How does 12-month continuous eligibility improve children’s health?
Children who have health insurance continuously throughout the year are more likely to have better health. Guaranteeing ongoing coverage ensures that children can receive appropriate preventive care, stay up to date on well-child visits and immunizations, fill their monthly prescriptions, and receive timely treatment for any health issues that arise. Stable coverage also enables providers to establish relationships with children and their parents and to track their health and development.
In contrast, when children experience gaps in health insurance coverage, they are less likely to have access to medical care. Interruptions in coverage can mean that children skip or delay a doctor’s visit or a prescriptions refill. People experiencing gaps in Medicaid coverage often experience serious health problems, while continuous Medicaid coverage is related to better health.
How will continuous eligibility help children with special health care needs?
According to Department of Health analysis, Medicaid children who are blind or disabled have one of the lowest average lengths of Medicaid eligiblity, compared to other eligibility categories. This suggests that children who are blind or disabled may be experiencing disruptions in care or coverage. A policy of 12-month continuous would allow all children, including those who are blind of disabled, to have continous health coverage.
How will continuous eligibility improve health plan accountability and value?
Continuous eligibility allows health plans to more accurately measure the quality of children’s health services and initiate program improvement strategies. Continuous eligibility improves health plan accountability. Health plans use a set of tools, called HEDIS measures (the Healthcare Effectiveness Data and Information Set), to assess their performance on health care and service. HEDIS measures require a one-year standard of continuous enrollment data. Children experiencing churn are not captured; HEDIS does not reflect the full make-up of children receiving care. Continuous eligibility leads to more comprehensive program improvement targets and better health care value for enrollees.
Why should Utah implement 12-month continuous eligibility now?
Despite declines in overall uninsured rates, Utah still has one of the highest rates of uninsured children in the nation. Continuous eligibility is a recognized best practice for states to lower their uninsured rate, improve program accountability and value, and assure vulnerable children get the best care.
Continuous eligibility helps retain children with low enrollment rates, including Hispanic children. Hispanic children are more likely to experience churn because of a change in their family’s temporary income status. At least 31% of Hispanic children have parents who lack year-round employment, compared to 18% of White children. Utah has the highest rate of uninsured Hispanic children in the nation. Programs that help children maintain continuous coverage, once they are enrolled, will reduce ethnic health disparities.
Health care leaders and officials urge states to adopt continuous eligibility as one of the top strategies to retain children in insurance programs and strengthen continuity of care.
12-month continuous eligibility is a critical way to make sure that Utah children have health insurance the entire year. All children should have access to health care without gaps or disruptions in coverage.
Printer-friendly Version:
![]() Support 12-Month Continuous Eligibility for Utah Kids with Medicaid
Support 12-Month Continuous Eligibility for Utah Kids with Medicaid
Photo Credit: © Talanis | Dreamstime.com - Family Under The Rain Photo
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor.