H.R. 1 and the Future of Health Care for Utah Families
Earlier this month, H.R. 1 was passed and signed into law, bringing widespread impacts to families across the nation in areas such as education, taxes, immigration, and health care. The passage of H.R. 1 (‘OBBB’) represents a significant shift in federal health policy, bringing forth new and consequential changes.
According to the Congressional Budget Office, the bill would cut Medicaid and CHIP spending by $1 trillion over the next ten years. An estimated 188,000 Utahns are at risk of losing their health coverage through Medicaid and the federal marketplace. Many of the health-related provisions in the final bill will impact Utah families' ability to receive consistent and affordable care, all while introducing new administrative barriers that will result in thousands losing coverage.
While implementation dates for each of these changes vary, families will no doubt feel the effects of the changes in the coming days, months, and years. Although we are disappointed in the passage of H.R. 1, we remain hopeful in the opportunity for community organizations, state leaders, and advocates to come together and push for policies that center children and families. We remain vigilant in our strong belief that when all children have access to high-quality healthcare, families thrive, communities grow, and our state becomes stronger.
Key Resources
H.R. 1 Provisions: Utah Impact Info Sheets
Download our Impact Sheet below for a complete overview of how each provision of HR1 will impact Utah families, including key details, projected numbers, and timelines for implementation.
H.R.1 Provisions: Timeline Chart
See our chart for a snapshot of the provisions that will impact Utah immigrant families with implementation dates, impacted entities, and sections of the bill, and other key data.
What Utah Families Can Expect
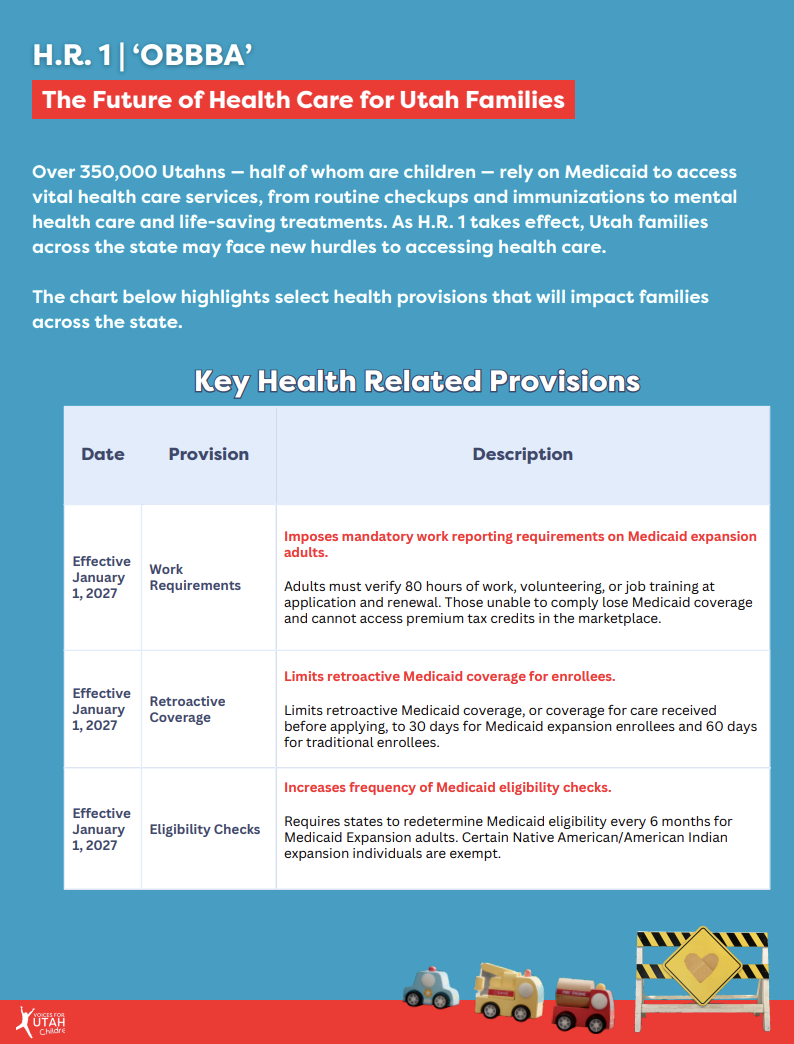
The changes to Medicaid and CHIP create new obstacles for parents, including work requirements if they have children over the age of 14, higher monthly premiums, and more frequent eligibility checks, which means more paperwork, more confusion, and a greater chance of losing coverage due to administrative issues. The following provisions are not meant to be all-encompassing but offer a look into the immediate impact they will have on Utahns.
Work Requirements
A particularly significant provision emerging from H.R. 1 is the adoption of work requirements. Utah will have to implement a work reporting requirement as a condition of eligibility for the Medicaid expansion population (those in the 19-64 age range) beginning no later than December 31, 2026. This means that in order to receive health coverage, an adult/parent has to meet work reporting requirements first. The state has to confirm that they met those requirements for at least one full consecutive month before applying.
Work requirements may be satisfied by providing proof of at least 80 hours of work per month, community service, participation in a work program, or enrolled in an educational program at least part time (or a combination of these). Despite both optional and mandatory exemptions, the burden of proof still falls on individuals. Although certain groups are excluded (see table below), parents with children over the age of 14 will be required to meet the work reporting requirements.
Nearly 20,000 Utah parents are part of the expansion group. Studies continually show that when parents have coverage, children are more likely to be insured and receive care. The potential loss of coverage for both children and their parents jeopardizes children’s long term health and development. Work requirements only add hurdles for parents' coverage and safety.
Eligibility Checks
Another change Utah parents and adults on Medicaid will experience include changes to eligibility checks. Utah will be required to conduct more frequent Medicaid eligibility every 6 months, rather than once a year for individuals enrolled in Medicaid Expansion. Such eligibility checks will push people off Medicaid coverage for failure to comply with unnecessary and burdensome paperwork requirements, even if they still qualify.
Cost Sharing
The bill also imposes new cost-sharing requirements that could create real barriers to care for low-income individuals. Adults with incomes over 100% of the federal poverty level would now face mandatory cost-sharing of up to $35 per visit or as much as $1,000 per year for someone earning around $15,000 annually.* This effectively creates a financial barrier to care for low-income adults enrolled through the ACA Medicaid expansion. For Utah families, this means that even with coverage, the cost of seeing a doctor or getting needed care could become unaffordable, leading many to delay or skip care altogether.
As healthcare costs continue to rise, even relatively small levels of cost-sharing can discourage people from seeking timely care, especially when every dollar counts. The bill does exempt services provided by federally qualified health centers, behavioral health clinics, and rural health clinics from these cost-sharing requirements, but the overall impact still risks pushing coverage further out of reach for many.
*The bill maintains the 5% family income cap on out-of-pocket costs.
Immigrant and Health Related Provisions
In addition, the bill makes drastic changes to immigrant communities' ability to access care. Under new rules, Medicaid coverage would only be allowed for people with permanent residency (still subject to a 5 year waiting period), Cuban and Haitian entrants, and those living under a Compact of Free Association. All others would be excluded, including refugees, asylees, survivors of trafficking and more. For a full list of immigration statuses, see table below.
Earlier provisions of great concern included a 10% FMAP penalty to states’ ACA Medicaid federal match rate for using state-only funds to provide coverage to immigrant groups — a change that would have impacted our State CHIP program — and a provision that would have made the 90-day reasonable opportunity period optional. This period allows Medicaid beneficiaries to receive coverage while submitting and verifying citizenship or immigration documents. Ultimately, both provisions were removed following the Senate Parliamentarian’s ruling that they, among others, violated the Byrd Rule, meaning they were deemed unrelated to the budget and therefore could not be included in the final bill.
The bill also eliminates ACA premium tax credit eligibility for most lawfully present immigrants and ends the exemption that allowed people earning below 100% of the federal poverty level to access ACA coverage. This means immigrant families will lose critical financial support to afford health insurance, making it much harder for them to get and keep coverage.
For an in-depth analysis of the H.R. 1 immigration provisions that will impact Utah families, click here.
What does this mean for Utah children and families?
In Utah, nearly 175,000 children rely on Medicaid and CHIP to cover doctor visits, immunizations, mental health care, dental services, home- and community-based care, and much more. Medicaid plays a vital role in supporting a child’s healthy development, but H.R. 1 adds layers of unnecessary red tape that threaten children’s ability to access consistent and affordable care especially during their most critical developmental years.
When we talk about Utah’s future and our declining birth rate we also have to talk about how these funding cuts will harm families with young children, pregnant women, and low-income households across the state. Without the support Medicaid provides, the question of “Where will families go for prenatal and delivery care?” becomes a very real concern.
At the same time, new cost-sharing requirements create steep financial barriers for low-income families, even those with coverage. When every dollar matters, these added costs can force families to delay or skip needed care, putting their health and stability at risk.
And for Utah’s mixed-status households and immigrant communities, this means fewer options, more fear, and growing inequities in health access and outcomes.
Together for Utah Families
The passage of H.R. 1 reinforces the urgent need for all of us who believe in a healthier future for Utah families to take action. These changes are not abstract; they will show up in doctor’s offices that parents can no longer afford, in missed vaccinations, untreated conditions, and growing anxiety for families navigating confusing new requirements.
But there is still work we can do. Community organizations, state leaders, and advocates must continue to fight for policies that center the health and well-being of children and families. We are committed to amplifying family voices, holding decision-makers accountable, and pushing for solutions that protect access to quality care for every Utah child.












